Jaundice
Introduction
Jaundice is a complex clinical syndrome characterized by the yellow discoloration of the skin, sclerae, and mucous membranes due to elevated serum bilirubin levels exceeding 2 to 3 mg/dL. Bilirubin, a tetrapyrrolic bile pigment, is formed during the catabolism of heme derived from senescent erythrocytes. The condition signals an underlying disorder in bilirubin metabolism, transport, or excretion, often linked to pre-hepatic, hepatic, or post-hepatic etiologies.
Historical Context
The recognition of jaundice can be traced back to ancient civilizations. It was meticulously documented in Egyptian papyri and addressed in Hippocratic writings. The term "jaundice" is derived from the French word "jaune," meaning yellow. Early interpretations attributed it to humoral imbalances. With advancements in hepatology, molecular biology, and imaging technology during the 19th and 20th centuries, our understanding of bilirubin metabolism and its pathological manifestations significantly improved.
Essential Anatomy and Physiology
- Liver: The central organ for bilirubin metabolism, where hepatocytes uptake unconjugated bilirubin and conjugate it with glucuronic acid via UDP-glucuronosyltransferase for excretion.
- Biliary System: Comprising intrahepatic and extrahepatic bile ducts, gallbladder, and sphincter of Oddi, essential for bile and bilirubin transport.
- Spleen: Plays a pivotal role in erythrocyte turnover and heme release.
- Kupffer Cells: Hepatic macrophages responsible for degrading hemoglobin into biliverdin, a precursor of bilirubin.
- Enterohepatic Circulation: Facilitates bile salt and bilirubin metabolite reabsorption, maintaining bilirubin homeostasis.
Types or Classification
- Pre-hepatic Jaundice: Caused by excessive hemolysis, resulting in increased unconjugated bilirubin.
- Hepatic Jaundice: Impaired hepatic uptake, conjugation, or excretion of bilirubin due to liver diseases such as hepatitis and cirrhosis.
- Post-hepatic (Obstructive) Jaundice: Bile duct obstructions prevent bilirubin excretion.
Pathophysiology
- Pre-hepatic: Increased erythrocyte lysis leads to unconjugated hyperbilirubinemia.
- Hepatic: Hepatocyte dysfunction compromises bilirubin uptake and conjugation, resulting in mixed hyperbilirubinemia.
- Post-hepatic: Biliary obstruction causes reflux of conjugated bilirubin into systemic circulation.
 |
| Causes of intrahepatic and extrahepatic jaundice |
- Yellow skin and sclera: Hallmark of elevated bilirubin.
- Dark urine: Indicates high conjugated bilirubin.
- Acholic stools: Suggests bile duct obstruction.
- Pruritus: Common in cholestatic jaundice.
- Systemic symptoms: Include malaise, anorexia, and abdominal discomfort.
Cardinal Signs and Symptoms
- Scleral Icterus: Early indicator of jaundice.
- Dark urine and pale stools: Hallmark of obstructive jaundice.
- Hepatomegaly: Suggestive of liver disease.
- Pruritus: Due to bile salt deposition.
Diagnostic Approach
- Clinical Evaluation: Thorough history and physical examination.
- Laboratory Investigations:
- Bilirubin Levels: Total, direct, and indirect bilirubin assays.
- Liver Function Tests (LFTs): ALT, AST, ALP, and GGT.
- Hemolysis Markers: LDH, haptoglobin, and reticulocyte count.
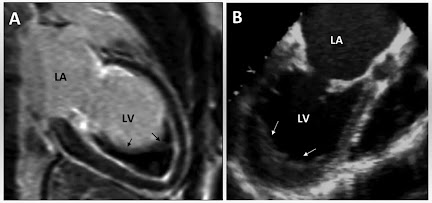
- Imaging Modalities:
- Ultrasound: Detects biliary obstruction.
- CT and MRI: Provides detailed anatomical visualization.
- MRCP: Non-invasive biliary tree imaging.
- Histopathology: Liver biopsy for definitive hepatic jaundice diagnosis.
Differential Diagnosis
- Carotenemia: Yellow skin without scleral involvement.
- Gilbert’s Syndrome: Benign hereditary hyperbilirubinemia.
- Viral Hepatitis: Hepatic inflammation with elevated transaminases.
- Primary Biliary Cirrhosis: Autoimmune cholestatic liver disease.
- Drug-Induced Liver Injury (DILI): Hepatotoxicity from medications.
Comparative Analysis of Jaundice Types
|
Feature |
Pre-Hepatic |
Hepatic |
Post-Hepatic |
|
Etiology |
Hemolysis |
Liver disease |
Bile duct obstruction |
|
Bilirubin Type |
Unconjugated |
Mixed |
Conjugated |
|
Stool Color |
Normal |
Pale |
Pale |
|
Urine Color |
Normal |
Dark |
Dark |
|
Pruritus |
Rare |
Common |
Severe |
Therapeutic Management
Allopathic Medicine
- Pre-hepatic:
- Blood transfusions for severe anemia.
- Glucocorticoids for autoimmune hemolysis.
- Hepatic:
- Antiviral Therapy: Tenofovir (300 mg daily) for chronic hepatitis B.
- Immunosuppressants: Prednisolone for autoimmune hepatitis.
- Liver Transplant: For end-stage cirrhosis.
- Post-hepatic:
- ERCP: Bile duct stenting.
- Cholecystectomy: Gallstone removal.
- Oncological Surgery: Tumor resection.
Homeopathic Medicine
- Chelidonium majus: 30C, three times daily for biliary disorders.
- Carduus marianus: 6X potency for hepatic detoxification.
- Nux Vomica: 30C for associated gastrointestinal complaints.
Unani Medicine
- Sharbat Banafsha: 10 ml twice daily for liver detox.
- Jawarish Jalinoos: 5 grams after meals.
- Majun Dabidul Ward: 5 grams twice daily for liver inflammation.
- Arq Mako: 125 ml twice daily.
Dietary Recommendations
- Include:
- Antioxidant-rich foods (berries, green tea).
- Hydration with coconut water and herbal teas.
- Low-fat dairy and whole grains.
- Avoid:
- Alcohol, fried foods, and red meat.
- Processed foods high in preservatives.
Adjunctive Therapies
- Phototherapy: Standard for neonatal jaundice.
- Ayurvedic Panchakarma: Liver detox procedures.
- Acupuncture: Symptom alleviation.
Surgical Interventions
- Cholecystectomy: For gallbladder stones.
- Biliary Stenting: To alleviate ductal obstruction.
- Liver Transplant: For irreversible hepatic failure.
- Tumor Resection: Oncological indications.
 |
| Clinical features and complications of cholestatic jaundice |
Complications
- Progression to chronic liver disease.
- Hepatic encephalopathy.
- Coagulopathy and bleeding disorders.
- Biliary cirrhosis.
- Acute renal failure.
- Sepsis in cholestatic jaundice.
Recent Advances
Emerging treatments in gene therapy and regenerative medicine show promise for conditions underlying jaundice. Advances in artificial liver support systems are undergoing clinical trials. Additionally, bile acid-binding agents have demonstrated efficacy in managing pruritus associated with cholestatic jaundice. Biomarker research is improving diagnostic precision and personalized therapy.
Summary
Jaundice, indicative of bilirubin metabolic dysregulation, necessitates a multidisciplinary approach encompassing diagnosis, medical, surgical, and supportive therapies. Recent innovations in therapeutic strategies hold promise for enhancing clinical outcomes.
References
- Friedman, L. S., & Keeffe, E. B. (2014). Handbook of Liver Disease. Elsevier.
- Sherlock, S., & Dooley, J. (2011). Diseases of the Liver and Biliary System. Wiley-Blackwell.
- Mayo Clinic. "Jaundice Overview." Retrieved from www.mayoclinic.org.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). "Liver Disease Information." www.niddk.nih.gov.
- WHO Guidelines for Hepatitis and Liver Disease Management. www.who.int.
- Kumar, P., & Clark, M. (2017). Clinical Medicine. Elsevier.





No comments:
Post a Comment
Please do not enter any spam link in the comment box