We offer topic-wise short notes and medical books to support medical students in their studies.
Endomyocardial Fibrosis
Endocardial Fibroelastosis
Endocardial Fibroelastosis
 |
| Image source Google |
Cardiac Amyloidosis
Cardiac Amyloidosis: An In-Depth Analysis
Cardiac amyloidosis is a progressive and life-threatening disorder characterised by the deposition of misfolded amyloid fibrils within the myocardium. This pathological protein accumulation results in increased myocardial stiffness, diastolic dysfunction, and, ultimately, heart failure. Due to its nonspecific clinical manifestations, cardiac amyloidosis often remains undiagnosed until advanced stages, highlighting the necessity for heightened clinical awareness and improved diagnostic methodologies.
 |
| Image source Google |
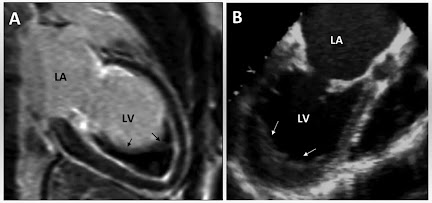
Dilated Cardiomyopathy
Idiopathic Dilated or Congestive Cardiomyopathy: A Comprehensive Guide
Idiopathic dilated or congestive cardiomyopathy is a heart condition that weakens and enlarges the heart muscle, impairing its ability to pump blood effectively. In simple terms, it’s like the heart becoming overstretched and losing its strength, making it harder for the body to receive the oxygen-rich blood it needs. Globally, idiopathic dilated or congestive cardiomyopathy affects millions, with estimates suggesting it accounts for approximately 25% of all cases of heart failure. Its significance lies in its profound impact on life expectancy and quality of life. Patients with idiopathic dilated or congestive cardiomyopathy often face challenges such as fatigue, shortness of breath, and even sudden cardiac arrest if left untreated. Understanding this disease is crucial for early detection and effective management.
 |
| Image source Google |
 |
| Image source Google |
Inflammation
Inflammation: Etiology, Pathophysiology, Clinical Manifestations, and Evidence-Based Interventions
Inflammation constitutes a complex biological response to noxious stimuli, encompassing infection, tissue injury, and immune dysregulation. While acute inflammation is integral to tissue homeostasis and repair, persistent or dysregulated inflammation has been implicated in the pathogenesis of numerous chronic diseases, including cardiovascular disease, metabolic disorders, and autoimmune conditions. This article elucidates the multifactorial causes of inflammation, delineates its clinical presentation, and examines both natural and medical modalities for mitigating its adverse sequelae.
 |
| Image source Google |
Encephalitis
Encephalitis
Synonyms
- Brain Inflammation
- Acute Viral Encephalitis
- Infectious Encephalitis
- Autoimmune Encephalitis
- Cerebral Infection
- Neuroinflammation
Introduction and Definition
Encephalitis is a severe, often life-threatening, inflammatory condition of the brain, typically resulting from viral infections, autoimmune reactions, or, in rarer cases, bacterial and fungal pathogens. The pathological hallmark of encephalitis is extensive neuroinflammation leading to neuronal dysfunction, cerebral edema, and, in severe cases, irreversible neurological sequelae. Given the heterogeneity in etiology and clinical presentation, accurate and timely diagnosis is imperative to optimize therapeutic interventions and reduce morbidity and mortality.
Hyperbilirubinemia
Jaundice
Introduction
Jaundice is a complex clinical syndrome characterized by the yellow discoloration of the skin, sclerae, and mucous membranes due to elevated serum bilirubin levels exceeding 2 to 3 mg/dL. Bilirubin, a tetrapyrrolic bile pigment, is formed during the catabolism of heme derived from senescent erythrocytes. The condition signals an underlying disorder in bilirubin metabolism, transport, or excretion, often linked to pre-hepatic, hepatic, or post-hepatic etiologies.
Stomach inflammation
Gastritis
Also known as Stomach inflammation, Gastric mucosal inflammation, Gastric irritation. Gastritis refers to the inflammation, irritation, or erosion of the gastric mucosa (the lining of the stomach). It can occur suddenly (acute gastritis) or gradually over time (chronic gastritis). The condition may be caused by various factors, including infections, medications, or autoimmune disorders.
Sweet syndrome
Sweet Syndrome (Acute Febrile Neutrophilic Dermatosis)
What is Sweet Syndrome?
Sweet Syndrome is a skin condition that causes painful, red or purple bumps and patches. It usually appears on the face, neck, and arms, and is often accompanied by fever and high levels of neutrophils in the blood.
Dengue Fever
DENGUE FEVER
Contents:
- Introduction
- Clinical presentation
- Diagnosis
- Treatment
- Diet
Introduction:
- Dengue fever is a viral infection caused by dengue virus.
- Dengue virus is an RNA virus of genus flavi virus.
- —There are four serotypes dengue virus that is DENV-1, DENV-2, DENV-3, DENV-4
-
—Dengue virus
transmitted by Aedes aegypti mosquito
| Aedes aegypti mosquito |
Aedes aegypti mosquito known to transmit Dengue virus, Yellow fever virus, Chikungunya virus, and Zika virus and it also suggest as a potential vector of Venezuelan Equine Encephalitis virus and studies shown it is capable to transmit West Nile virus as well.
Clinical Presentation:
Divides into 4 categories :
- Dengue without warning sign
- Dengue with warning sign
- Severe dengue / dengue hemorrhagic fever
- Dengue shock syndrome
- Not all patient goes in all these phases.—
- Majority of patient develops dengue without warning sign and they cure self or general treatment.
- But few patients who are not manage properly or the patient who are immunocompromised and who have weak immune system, they can progress from dengue without warning sign to dengue shock syndrome.
- Incubation period 4-10 days (2-14 days)
- —High grade fever 40˚C (104˚f)
- Severe headache
- Retro orbital pain
- Myalgia, arthralgia (break bone fever)
- Maculopapular widespread rashes.
- Generalised lymphadenopathy.
- —Pt. with severe comorbidities
- —Infants less than 1 year of age
- —History of previous or recurrent dengue infection.
- Abdominal pain with or without tenderness.
- Persistent vomiting (>3 times in 24 hours)
- —Bleeding from nose or gums.
- —Blood in vomiting or blood in stool or blood in urine.
- —Lethargy, restlessness, irritable.
- —Enlarge liver > 2 cm
Severe Dengue / Dengue haemorrhagic fever
Re-infected with different serotype
This phase begins after fever subside
—Temperature (hypothermia to second fever spike)
—Plasma leak resulting in pleural effusion, ascites, haematocrit drops
—Hemorrhagic manifestations such as gingival bleed, epistaxis, petechiae, ecchymosis, purpura, thrombocytopenia,
—Severe organ involvement like hepatomegaly, liver failure
—Changes in mental status - confusion
| Petechiae and Purpura |
| Ecchymosis |
| Gingival Bleeding |
Dengue Shock Syndrome
Severe hemorrhagic dengue
+
Shock (circulatory collapse)
| When test become positive |
Tourniquet applied to arm. Inflated to a point b/w systolic and diastolic pressure for 5 minutes.
Positive test : If 10 or more petechiae appear per square inch on forearm.
Treatment Approache
Don’t do this
You can do this
Dengue without warning sign Treatment approach
Dengue with warning sign treatment approache
Severe Dengue / Dengue haemorrhagic fever
Check haematocrit level
DECREASING
Or